Read the abstract of this interesting article:
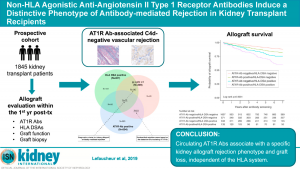
Anti-angiotensin II type 1 receptor (AT1R) antibodies have been associated with allograft rejection. We hypothesized that circulating AT1R antibodies might identify kidney transplant recipients at increased risk of allograft rejection and loss who are not identified by the HLA system. We prospectively enrolled 1845 kidney transplant recipients from two centers. Donor-specific HLA antibodies (DSAs) and AT1R antibodies were measured at the time of the first acute rejection episode or at 1 year post-transplant. Allograft biopsy was performed to evaluate the rejection phenotype and to assess for endothelial activation.
AT1R antibodies were associated with an increased risk of allograft loss. Participants with AT1R antibodies had a higher incidence of antibody-mediated rejection (AMR) compared with participants without AT1R antibodies. Among 77 participants with histological features of AMR but without DSAs, 51 (66.2%) had AT1R antibodies.
Compared to participants with prototypical DSA-mediated rejection, those with AT1R antibody-associated rejection had a higher prevalence of hypertension, more vascular rejection with arterial inflammation, higher levels of endothelial-associated transcripts, and lack of complement deposition in allograft capillaries.
Thus, AT1R antibodies may identify kidney transplant recipients at high risk of allograft rejection and loss, independent of the HLA system. Recognition of complement-independent AT1R antibody-mediated vascular rejection could lead to the development of new treatment strategies to improve allograft survival.
Read more about it.